Two leading US university hospitals, Duke University and Vanderbilt University, have developed innovative methods to recover hearts for transplant from donors who die after circulatory death, a move experts say could significantly expand access to lifesaving heart transplants for both adults and infants.
Published in the New England Journal of Medicine, the breakthrough techniques aim to safely retrieve donor hearts that would typically go unused due to a time lapse between cardiac arrest and organ removal, a key challenge in donation after circulatory death (DCD).
“These DCD hearts work just as well as hearts from brain-dead donors,” said Dr. Aaron Williams of Vanderbilt, whose team successfully transplanted DCD hearts into three adult men. Meanwhile, Duke surgeons performed a landmark transplant on a 3-month-old infant using a new method that could be more widely adopted in paediatric cases.
Also Read | Heart attack survival rates soar in US, but other cardiac threats rise
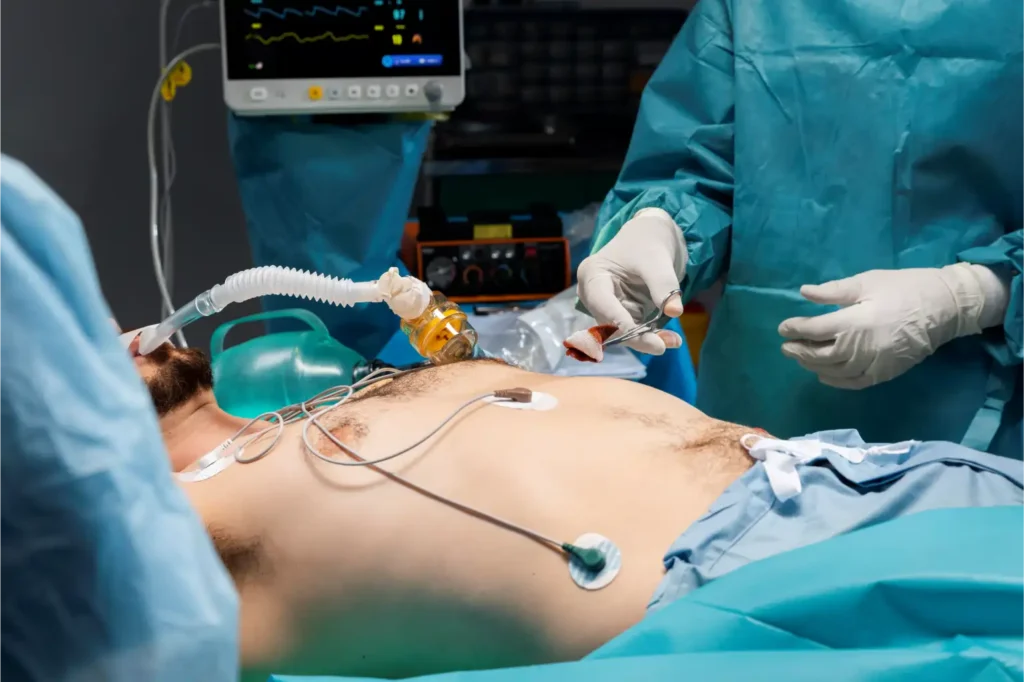
Currently, most heart transplants rely on donors declared brain dead, where the heart continues to beat via ventilator support until it’s removed. In contrast, DCD involves donors who have suffered catastrophic brain injury but haven’t met full brain death criteria—once life support is withdrawn, the heart stops, and oxygen deprivation begins.
While kidneys and livers can often be salvaged post-circulatory death, hearts are highly sensitive to oxygen loss, making their viability uncertain. To work around these barriers, Duke and Vanderbilt teams devised alternative approaches.
Duke’s method, led by Dr. Joseph Turek, involves briefly assessing the donor heart’s function on a sterile table in the operating room, not inside a machine. This low-tech approach was tested on piglets before being used in a real case, where the heart of a 1-month-old donor was successfully transplanted into a critically ill 3-month-old infant.
Vanderbilt’s approach uses a nutrient-rich cold preservation solution to protect the heart before removal, similar to the process used for brain-dead donors. It avoids both reanimation and expensive machines, and has been used in about 25 transplants so far.








