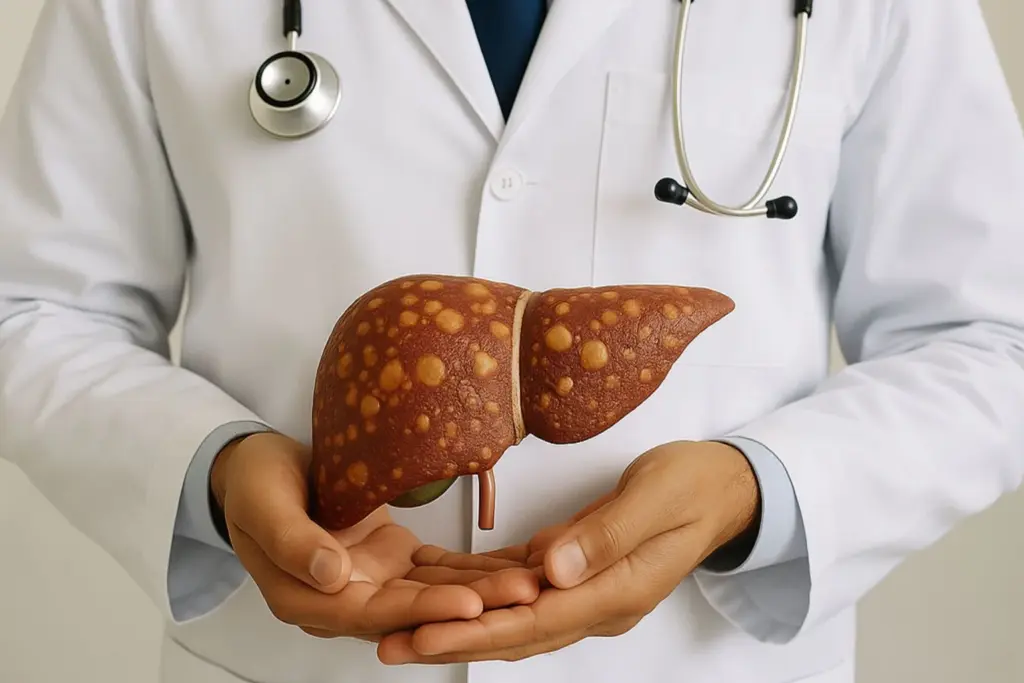
Fatty liver: Fat in the liver doesn’t come from one source. Some livers are injured by alcohol; others by metabolic stress (weight, insulin resistance, lipids). The labels differ, but the day-to-day care looks remarkably similar.
This guide explains what separates alcoholic fatty liver from non-alcoholic fatty liver, where they overlap, and how to protect your liver starting today.
Also Read | Our Expert Article: Dr Pratik Savaj On Life Beyond HIV & Modern Treatments
Two pathways to a fatty liver:
- Alcohol-associated liver disease (ALD): Fat, inflammation, and scarring due to harmful alcohol use. Stopping alcohol fully improves survival at every stage, including cirrhosis.
- Non-alcoholic fatty liver disease (NAFLD): Fatty liver linked to metabolic factors (overweight/obesity, type 2 diabetes, dyslipidaemia, hypertension). The global community now uses the updated term MASLD (metabolic dysfunction–associated steatotic liver disease), but most patients still recognise “NAFLD,” so we use both terms.
Who is at risk of fatty liver?
- ALD: Any sustained harmful intake or repeated binge patterns. Genetics and poor nutrition worsen the risk. Complete abstinence is the single most effective treatment.
- NAFLD/MASLD: Higher with central obesity, insulin resistance/diabetes, high triglycerides, high blood pressure, even in some “lean” people.
How can both alcohol and non-alcoholic fatty liver progress?
Both conditions can progress from simple steatosis (fat) to steatohepatitis (fat plus inflammation), then to fibrosis, cirrhosis, and finally liver cancer (HCC). Anyone with cirrhosis, whatever the cause, should undergo ultrasound-based HCC surveillance every 6 months.
Diagnosing and staging: What to expect
- Blood tests (LFTs), metabolic profile, and viral hepatitis screening.
- Ultrasound can suggest fatty change but does not stage disease; we increasingly use non-invasive fibrosis tools: FIB-4 (age, AST, ALT, platelets) and elastography (FibroScan). Many patients can be risk-stratified without biopsy.
Different liver diseases, same core lifestyle prescription
- ALD: Ongoing alcohol drives inflammation, portal hypertension, malnutrition, and higher short-term decompensation risk. Abstinence changes the curve at all stages.
- NAFLD/MASLD: Tightly tied to cardiometabolic risk (heart disease, stroke). Managing weight, glucose, lipids, and BP is as important as the liver itself.
Fatty liver: Tips to take care
Alcohol:
- ALD: zero alcohol; no “safe” amount.
- NAFLD/MASLD: even “moderate” intake can worsen outcomes; the safe advice is to avoid alcohol.
Weight & activity:
Target 7–10% weight loss to improve liver fat and inflammation; =10% can regress scarring. Pair calorie control with 150–300 minutes/week of moderate activity plus resistance training.
Food pattern:
Emphasise vegetables, pulses, whole grains, nuts, lean protein; cut ultra-processed foods, sugary beverages, excess oils. Spread protein throughout the day; avoid late-night heavy meals (they can worsen reflux and glycaemia).
Metabolic health:
Tight control of diabetes, lipids, blood pressure; review medications that can injure the liver; vaccinate for hepatitis A & B if non-immune.
Monitoring:
Periodic FIB-4/elastography to track fibrosis; if cirrhosis, add 6-monthly HCC surveillance and variceal/ascites assessment per cirrhosis care checklists.
“Is there a tablet for fatty liver?”
Lifestyle remains first-line. Selected patients with biopsy-proven steatohepatitis may be considered for specific therapies, but these decisions are specialist-led and individualised; no pill replaces weight loss or alcohol abstinence.
Also Read | Our Expert Article: Dr Mukur Petrolwala On How Late-Night Gaming Affect Teen BP
When to see a doctor urgently?
Vomiting blood or black stools, yellowing of eyes/skin, drowsiness or confusion, increasing abdominal swelling, persistent unintentional weight loss, or severe muscle wasting, please seek care immediately.
ALD and NAFLD/MASLD arrive by different roads, but both respond to the same fundamentals: zero alcohol in ALD (and best avoided in NAFLD), weight and waist reduction, fitness, metabolic control, and regular monitoring. Done consistently, these steps change the liver’s trajectory, often dramatically.
Medical disclaimer: This article is for education, not a substitute for personal medical advice. Treatment varies by individual health status, please consult your own doctor for guidance.








