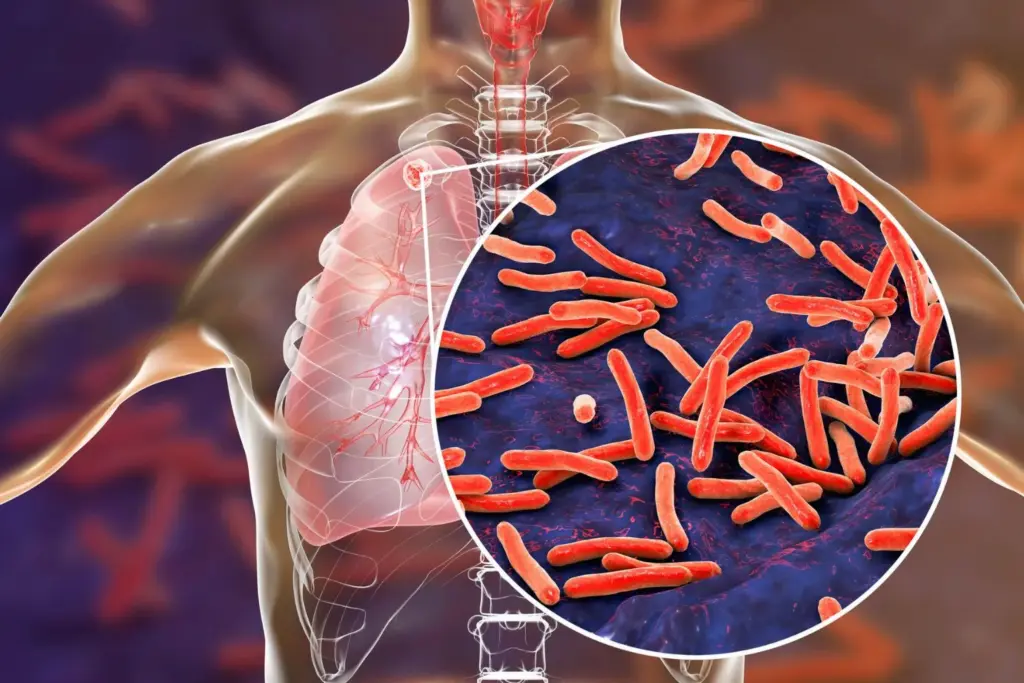
Tuberculosis bacteria: Researchers from IIT Bombay and Monash University have reported new clues on why tuberculosis bacteria can survive antibiotic treatment during dormancy, a state that often underpins long and difficult TB therapy.
In a study published in Chemical Science, the team found that TB-like bacteria become highly tolerant to antibiotics by remodelling the lipids in their outer membrane, making the barrier more rigid and harder for drugs to cross. The paper is titled “Decoding the role of mycobacterial lipid remodelling and membrane dynamics in antibiotic tolerance.”
Also Read | India’s TB cases fall 21%, nearly twice the global decline
Tuberculosis remains a major global threat. The disease affected an estimated 10.8 million people worldwide in 2023 and caused 1.25 million deaths. India continues to carry the highest burden, with recent national data showing improved diagnosis and treatment coverage.
Standard TB treatment typically lasts at least six months, partly because dormant bacteria can persist despite prolonged drug exposure. To understand the biology behind this tolerance, the researchers used Mycobacterium smegmatis, a harmless relative that mimics key TB behaviours but can be studied safely. They compared bacteria in an active growth phase with those in a late-stage condition that resembles dormancy.
Testing four TB drugs, rifabutin, moxifloxacin, amikacin and clarithromycin, the team found that dormant cells required two to ten times higher drug concentrations to suppress growth compared with active cells. Importantly, this reduced sensitivity was not tied to genetic resistance.
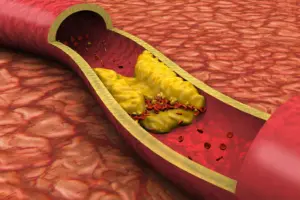
Advanced lipid profiling identified more than 270 membrane molecules and showed a clear shift in dormant cells towards long, waxy fatty acyls. These changes were associated with tighter lipid packing and lower membrane fluidity, reducing permeability. A sharp drop in cardiolipin, a lipid associated with maintaining membrane looseness, appeared to further strengthen the barrier.
The researchers said the findings suggest a potential strategy to boost TB therapy: combining antibiotics with agents that gently loosen the outer membrane. The team is now exploring antimicrobial peptides that may improve drug entry when used alongside existing treatments.
The next step will be to validate these results using the actual TB bacterium under higher biosafety conditions.